Feasibility, safety and clinical efficiency of optometric service pathways at primary and tertiary care level in Ampang, Malaysia
a pilot study
Abstract
Aim: To evaluate feasibility, safety, and clinical efficiency of optometrists in conducting diabetic retinopathy screening and ocular health screening.
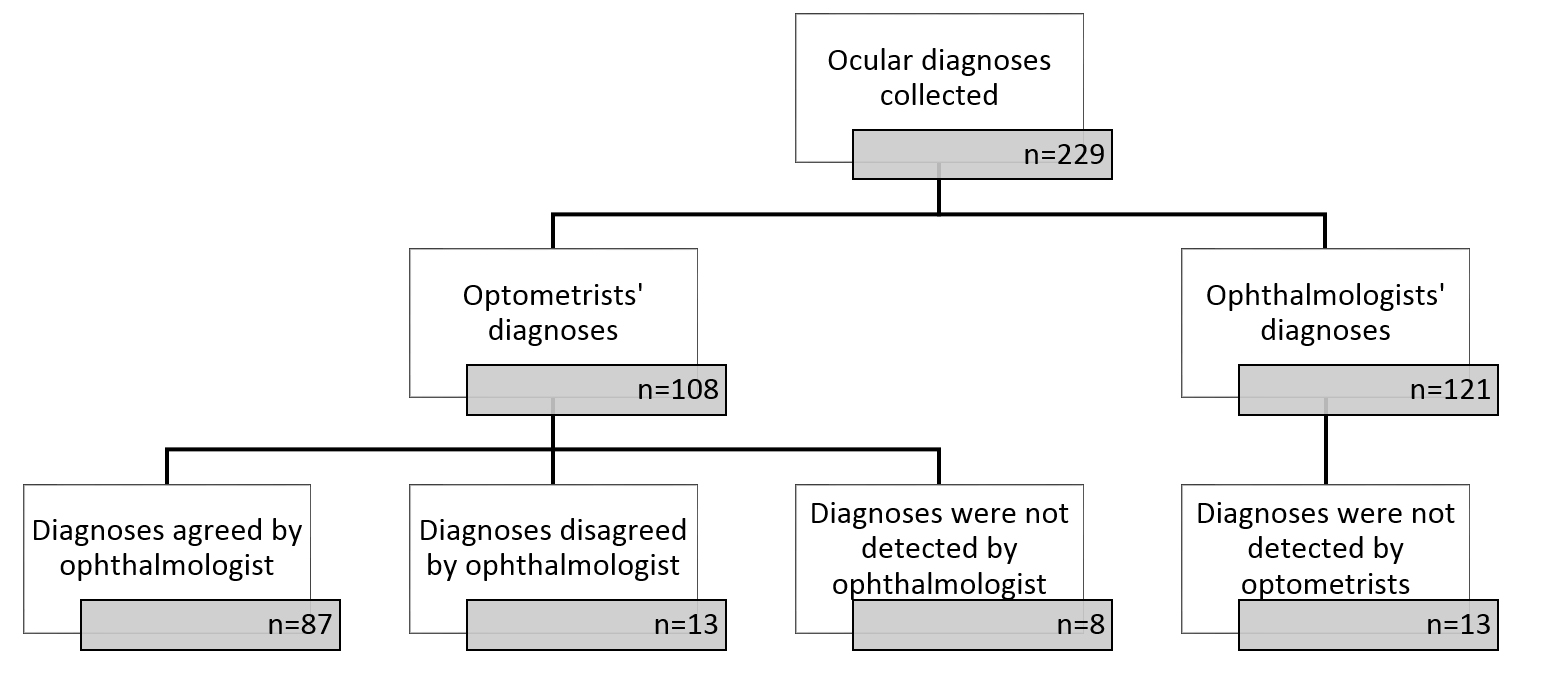
Methods: This was a prospective observational trial study of newly developed optometric service pathways established at a community health clinic for diabetic retinopathy screening and a hospital ophthalmology clinic for ocular health screening. The study was carried out to assess the feasibility and safety of eye examinations conducted by optometrists. Patients were examined by optometrists using a standard eye examination at both clinics and re-examined by ophthalmologists as the reference standard. Optometrists recorded diagnoses of ocular conditions and classified referral urgency for each patient and these were compared with the diagnoses made by ophthalmologists, who were masked to the optometrists’ findings.
Results: There was a high concordance of 87.0% (95% CI 80.4%-93.6%) for the diagnoses between the optometrists and ophthalmologists. Of 26 patients considered by the optometrists to need ophthalmology referral, 23 were agreed as such by the ophthalmologists, giving good agreement, κ = 0.76 (95% CI 0.53 -0.94) between the optometrists and ophthalmologists on referral classification. Agreement by the ophthalmologists for referral urgency classifications (very urgent/urgent or non-urgent) was very good (κ = 0.85, 95%CI 0.62-1.00).
Conclusions: Ocular health examination by optometrists using optometric-eyecare pathways is feasible and safe. Optometrists showed strong agreement with ophthalmologists when diagnosing patients who had a range of ocular conditions. Optometrists were also able to triage referrals and their urgency accurately, suggesting that they could play an extensive role as primary eye care providers, thus reducing unnecessary referrals to ophthalmology clinics.
References
2. Goh PP, Omar MA, Yusoff AF. Diabetic eye screening in Malaysia: findings from the National Health and Morbidity Survey 2006. Singapore Med J. 2010;51(8):631-634.
3. Hau S, Ehrlich D, Binstead K, Verma S. An evaluation of optometrists' ability to correctly identify and manage patients with ocular disease in the accident and emergency department of an eye hospital. Br J Ophthalmol. 2007;91(4):437-440.
4. Harper R, Creer R, Jackson J, et al. Scope of practice of optometrists working in the UK Hospital Eye Service: a national survey. Ophthalmic Physiol Opt.2016;36(2):197-206.
5. Sheen NJ, Fone D, Phillips CJ, Sparrow JM, Pointer JS, Wild JM. Novel optometrist-led all Wales primary eye-care services: evaluation of a prospective case series. Br J Ophthalmol. 2009;93:435-438.
6. Mohidin N, Hashim A. Amalan optometris di praktis swasta sekitar Kuala Lumpur dan Lembah Klang: Satu kajian awal (Optometric practice in private sector around Kuala Lumpur and Klang Valley: a preliminary study). Jurnal Sains Kesihatan Malaysia 2011; 9:29-34.
7. Tan KO, C Lam. Optometry graduates: are they practicing what they have learnt? In: World Conference on Optometry Education. 2010. Durban, South Africa.
8. Bourne RR, French KA, Chang L, Borman AD, Hingorani M, Newsom WD. Can a community optometrist-based referral refinement scheme reduce false-positive glaucoma hospital referrals without compromising quality of care? The community and hospital allied network glaucoma evaluation scheme (CHANGES). Eye 2010; 24(5):881-887.
9. Lockwood AJ, Kirwan JF, Ashleigh Z. Optometrists referrals for glaucoma assessment: a prospective survey of clinical data and outcomes. Eye. 2010;24(9):1515-1519.
10. De Souza N, Cui Y, Looi S, et al. The role of optometrists in India: An integral part of an eye health team. Indian J. Ophthalmol. 2012;60(5):401-405.
11. Sundling V, Gulbrandsen P, Straand J. Sensitivity and specificity of Norwegian optometrists' evaluation of diabetic retinopathy in single-field retinal images - a cross-sectional experimental study. BMC Health Serv Res. 2013;13(1):13-17.
12. Syam P, Rughani K, Vardy SJ, et al., The Peterborough scheme for community specialist optometrists in glaucoma: a feasibility study. Eye. 2010;24(7):1156-1164.
13. World Health Organization. Diseases of the eye and adnexa, international statistical classification of diseases and related health problems. 10th revision (ICD-10). 2007: Geneva.
14. Ministry of Health Malaysia, Clinical practice guidelines for screening of diabetic retinopathy. 2011; Percetakan Nasional Berhad: Putrajaya.
15. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1): 159-174.
16. Morris RW, Dunbar MT. Atypical presentation and review of the ICE syndrome. Optometry. 2004;75(1):13-25.
17. Laganowski HC, Kerr Muir MG, Hitchings RA. Glaucoma and the iridocorneal endothelial syndrome. Arch Ophthalmol. 1992;110(3):346-350.
18. Teekhasaenee C, Ritch R. Iridocorneal endothelial syndrome in Thai patients: clinical variations. Arch Ophthalmol. 2000;118(2):187-192.
19. Selvarajah S. An analysis of glaucoma patients seen at the General Hospital Kuala Lumpur over a five year period: 1986 to 1990. Med J Malaysia. 1998;53(1): 42-45.
20. Sergi M, Salerno DE, Rizzi M, et al., Prevalence of normal tension glaucoma in obstructive sleep apnea syndrome patients. J Glaucoma. 2007;16(1):42-46.
21. Myint J, Edgar DF, Murdoch IE, Lawrenson JG. The impact of postgraduate training on UK optometrists' clinical decision-making in glaucoma. Ophthalmic Physiol Opt.2014;34(3): 376-384.
22. Azuara-Blanco A, Burr J, Thomas R, Maclennan G, McPherson S. The accuracy of accredited glaucoma optometrists in the diagnosis and treatment recommendation for glaucoma. Br J Ophthalmol. 2007;91(12):1639-1643.
23. Parkins DJ, Edgar DF. Comparison of the effectiveness of two enhanced glaucoma referral schemes. Ophthalmic Physiol Opt. 2011;31(4):343-352.
24. Goh PP. Status of diabetic retinopathy among diabetics registered to the Diabetic Eye Registry, National Eye Database, 2007. Med J Malaysia. 2008; 63(Supplement C): 24-28.
25. Keat EL, Keat WK. Audit of diabetic retinopathy referrals to Penang Hospital, a tertiary Ophthalmology centre in Malaysia. Asian Journal of Ophthalmology 2009;11:17-19.
Copyright (c) 2019 Asian Journal of Ophthalmology

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication, with the work twelve (12) months after publication simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access).