Macular thickness in diabetic retinopathy without clinically significant macular edema
a prospective study
Abstract
Aim: To measure macular thickness by optical coherence tomography (OCT) in various grades of diabetic retinopathy with no clinically significant macular edema (CSME) and its comparison with non-diabetics.
Design: Prospective cross–sectional study.
Methods: Macular thickness was measured by OCT in 72 healthy volunteers (107 control eyes), 45 patients with mild and moderate non-proliferative diabetic retinopathy (NPDR) (78 eyes) and 37 patients with severe NPDR and proliferative diabetic retinopathy (PDR) (66 eyes). Patients with diabetic macular edema (DME) as assessed by stereoscopic evaluation or photographs were excluded. One-way ANOVA test to compare the mean thickness and Tukey's test for multiple comparison between groups were used.
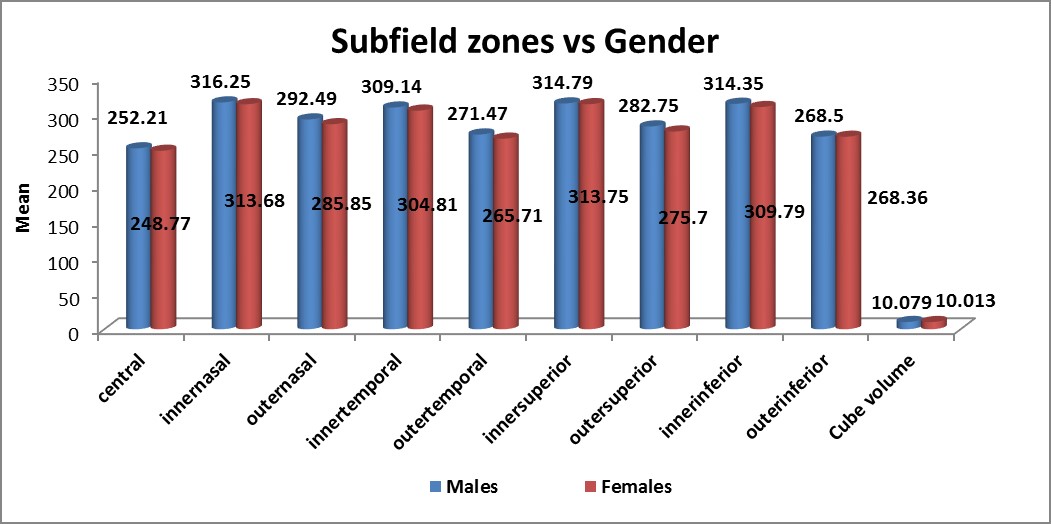
Results: Central subfield thickness (CST) was 238.57 ± 25.077 µm, 251.22 ± 24.649 µm, and 270.45 ± 28.956 µm in the three groups respectively. As the severity of retinopathy increased, the macular thickness significantly increased (p = < 0.001) in all the nine zones on OCT. There was a significant increase in CST noted in all the grades of retinopathy when compared with non-diabetics (p = 0.004, p = < 0.0001). No significant difference in macular thickness was noted between genders, irrespective of their groups (p = 0.72), or between the three groups in all the nine zones (p = 0.609).
Conclusion: There is a significant increase in CST in all grades of retinopathy, as well as with increasing severity of retinopathy when compared to non-diabetics. This warrants the need to obtain OCT measurements even in patients with moderate NPDR without CSME to rule out subclinical DME.
References
2. Brown JC, Solomon SD, Bressler SB, Schachat AP, DiBernardo C, Bressler NM. Detection of diabetic foveal edema contact lens biomicroscopy compared with optical coherence tomography. Arch Ophthalmol. 2004;122(3):330-335.
3. Pires I, Santos AR, Nunes S, Lobo C, Cunha-Vaz J. Subclinical macular edema as a predictor of progression to clinically significant macular edema in type 2 diabetes. Ophthalmologica. 2013;230(4):201–206. doi:10.1159/000354550.
4. Bressler NM, Miller KM, Beck RW, et al. Observational study of subclinical diabetic macular edema. Eye (Lond). 2012; 26(6): 833–840. doi:10.1038/eye.2012.53.
5. Early Treatment Diabetic Retinopathy Study Research Group. ETDRS report number 7: Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. Ophthalmology. 1991;98(5):741–756.
6. Wilkinson CP, Ferris FL, Klein RE, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110(9):1677-1682.
7. Browning DJ, Glassman AR, Aiello LP, et al. Optical coherence tomography measurements and analysis methods in optical coherence tomography studies of diabetic macular edema. Ophthalmology. 2008; 115(8): 1366–1371. doi:10.1016/j.ophtha.2007.12.004.
8. Chalam KV, Bressler SB, Edwards AR, et al. Retinal thickness in people with diabetes and minimal or no diabetic retinopathy: Heidelberg Spectralis optical coherence tomography. Invest Ophthalmol Vis Sci. 2012; 53(13):8154–8161. doi: 10.1167/iovs.12-10290.
9. Bressler SB, Edwards AR, Chalam KV, et al. Reproducibility of spectral domain optical coherence tomography retinal thickness measurements and conversion to equivalent time-domain metrics in diabetic macular edema. JAMA Ophthalmol. 2014;132(9):1113-1122. doi: 10.1001/jamaophthalmol.2014.1698.
10. Grover S, Murthy RK, Brar VS, Chalam KV. Normative data for macular thickness by high‑definition spectral domain optical coherence tomography (Spectralis). Am J Ophthalmol. 2009;148(2):266‑271.doi: 10.1016/j.ajo.2009.03.006.
11. Pournaras JA, Erginay A, Lazrak Z, Gaudric A, Massin P. Spectral domain optical coherence tomography in diabetic macular edema. Ophthalmic Surg Lasers Imaging. 2009;40:548-553.
12. Patel N, Chowdhury H, Leung R, Sivaprasad S. Sensitivity and specificity of time-domain versus spectral-domain optical coherence tomography in diabetic macular edema. Indian J Ophthalmol. 2013;61(5):208-212. doi:10.4103/0301-4738.99848.
13. Appukuttan B, Giridhar A, Gopalakrishnan M, Sivaprasad S. Normative spectral domain optical coherence tomography data on macular and retinal nerve fiber layer thickness in Indians. Indian J Ophthalmol 2014;62(3):316-321. doi:10.4103/0301-4738.116466.
14. Yang CS, Cheng CY, Lee FL, Hsu WM, Liu JH. Quantitative assessment of retinal thickness in diabetic patients with and without clinically significant macular edema using optical coherence tomography. Acta Ophthalmol Scand. 2001;79(3):266–270.
15. Goebel W, Kretzchmar-Gross T. Retinal thickness in diabetic retinopathy: a study using optical coherence tomography (OCT). Retina. 2002 Dec;22(6):759-767.
16. Browning DJ, Fraser CM, Clark S. The relationship of macular thickness to clinically graded diabetic retinopathy severity in eyes without clinically detected diabetic macular edema. Ophthalmology. 2008;115(3):533–539.
17. Sánchez-Tocino H, Alvarez-Vidal A, Maldonado MJ, Moreno-Montañés J, GarcÃa-Layana A. Retinal thickness study with optical coherence tomography in patients with diabetes. Invest Ophthalmol Vis Sci. 2002;43(5):1588-1594.
18. Hee MR, Puliafito CA, Duker JS et al. Topography of diabetic macular edema with optical coherence tomography. Ophthalmology 1998;105(2):360–370.
19. Estabrook EJ, Madhusudhana KC, Hannan SR, Newsom RS. Can optical coherence tomography predict the outcome of laser photocoagulation for diabetic macular edema? Ophthalmic Surg Lasers Imaging. 2007;38(6):478-483.
Copyright (c) 2018 Asian Journal of Ophthalmology

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication, with the work twelve (12) months after publication simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access).